MACRA Ready™ Features
QCDR Reporting
Your anesthesia practice’s best chance of receiving the maximum bonus from CMS (estimated at 5.67%) is QCDR reporting.
Analytics Dashboards
You’ll need to easily track, trend, and share details about performance, and Graphium’s MACRA Compliance, Organizational Scorecards, and Facility Scorecards allow you to do just that.
Joint Commission Reports
You and your anesthesia practice – as 3rd party hospital service providers – are required to have specific data on hand at all times for TJC certification. Everything you need is here in these quarterly reports.
Advanced Measures
Your practice is more than just average–and your reporting should be, too. You will exceed mere compliance with 7 reportable measures, 3 quality process measures, and 39 outcome measures.
OPPE Enabled
Your On-going Provider Professionalism Evaluation & credentialing data needs are already covered with Graphium’s MACRA Ready™ forms.
Operational Insight
You will enjoy an unprecedented view of your operational performance with over 14 additional reports, including productivity, efficiency, throughput, and staffing utilization.
Two Ways to Record MACRA Data
Choose any combination that best suits your practice.
You Can Digitize With
Graphium’s iOS App
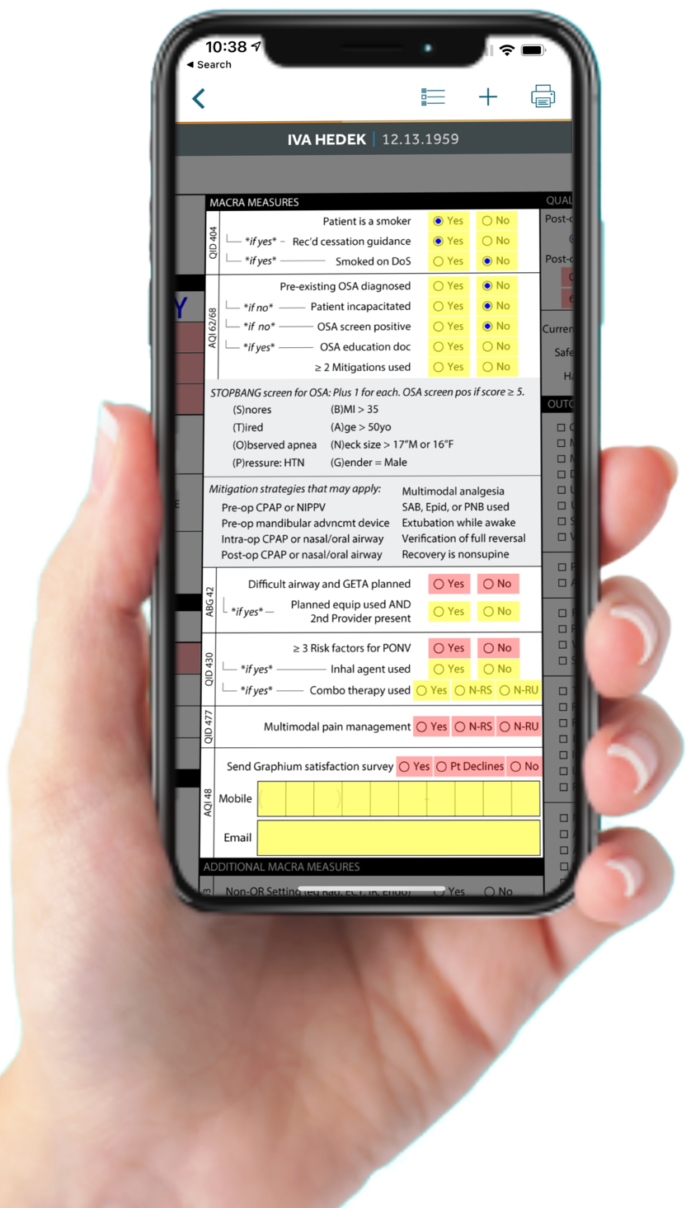
Your MACRA compliance is brought to life by mobile data entry on your iPhone or iPad. Your teams laborious compliance process becomes and invaluable quality program in just a few screen touches.
Or You Can
Use A Paper Record
You can get started as quickly as you can print a sheet of paper. These forms include all of the measures you need to collect for MACRA compliance. Fill one out for each case, fax or upload them to us, and we’ll take it from there.

